Angioplasty & Stents
Percutaneous Coronary Intervention (PCI)
Overview
In people with cardiovascular disease (CVD), a fatty substance called plaque gradually builds up in arteries throughout their body. It causes problems when the buildup is so great that it slows or stops the flow of blood through the arteries. Plaque that ruptures and breaks free, or a blood clot inside the artery, can clog an artery, potentially preventing vital organs and other parts of the body from getting the oxygen they need to work. This is where angioplasty and stenting plays a role.
Learn about angioplasty & stents in this animated video.
An angioplasty and stenting procedure is a treatment for CVD that's been performed for more than 45 years and is recognized as the best way to stop a heart attack in progress. This minimally invasive procedure can also be used to treat blocked arteries and restore the flow of blood for patients who are suffering from angina, stroke, peripheral artery disease (PAD), or renal artery stenosis (RAS). You also might hear doctors and other health care providers refer to angioplasty and stenting in the coronary arteries as “PCI,” which stands for percutaneous coronary intervention. It’s a procedure (intervention) performed in one or more arteries to the heart (coronary) through a puncture or small incision in the skin (percutaneous) rather than surgery.
Benefits of angioplasty and stenting
Treating blocked arteries with angioplasty and stenting can help with the following:
- Saving your life and reducing heart muscle damage during a heart attack by restoring blood flow to the heart
- Possibly offering immediate relief, or at least reducing, symptoms such as chest pain, shortness of breath, and fatigue, making you feel better and able to do more each day.
- Reducing your risk of having a stroke
- Improving the function of your kidneys
- Restoring blood flow to the legs to prevent gangrene and eliminate the need for amputation
Some patients with extensive blockage in their heart arteries clearly benefit more from open-heart surgery to restore blood flow to the heart. These patients have extensive blockage in all three major arteries or in an artery called the “left main.” In comparison to open-heart surgery, angioplasty and stenting is less invasive than surgery because the clogged or blocked artery is accessed from a tiny incision in the upper leg or the wrist. Angioplasty and stenting may allow you to recover more quickly than you would from surgery, which can also mean less time in the hospital and returning to your regular activities more quickly.
Stories of Hope and Recovery

Patient Story: Eugene received a percutaneous coronary intervention (PCI) for chronic total occlusion (CTO) with the care of an interventional cardiologist.
How does it work?
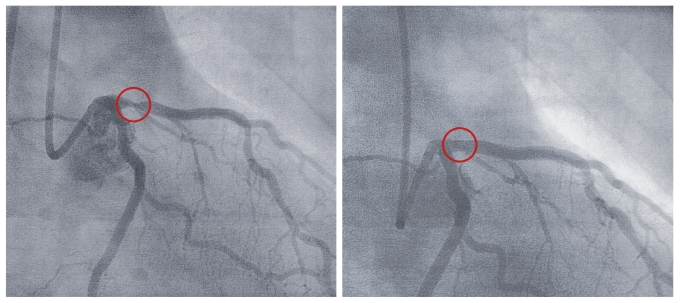
During angioplasty, an interventional cardiologist opens the clogged or blocked artery with the help of a very thin tube (a catheter) that is threaded through a blood vessel to the site of a blockage. The catheter has a balloon attached that expands to push away the material that’s causing the blockage. The balloon is deflated and is removed with the catheter, leaving behind an open blood vessel. To keep the artery from becoming renarrowed with plaque (called restenosis), your doctor may insert a metal, mesh tube called a stent. The stent is expanded into place to prop open the artery. Without a stent, an artery cleared by angioplasty could collapse, once again cutting off blood flow.
Because the procedure is performed via a small incision in the groin or wrist (rather than requiring major surgery), it’s considered a minimally invasive way to treat CVD and restore the flow of blood to the heart, brain, legs, or kidneys.