Pericarditis
Overview
Pericarditis is a condition in which the sac-like tissue (pericardium) that surrounds the heart becomes inflamed, swollen, or irritated. The amount of fluid that surrounds the heart within the pericardial sac can increase and cause a condition called a pericardial effusion.
Causes of pericarditis
There are several causes of pericarditis, but in many cases, doctors can’t determine the exact cause. Pericarditis can be caused by the following:
- Viral infections
- Bacterial infections
- Autoimmune diseases
- Kidney failure
- Medications that suppress the immune system
- Injury to the chest
Symptoms of Pericarditis
The most common symptom of pericarditis is sharp, stabbing chest pain, which is caused by friction from the inflamed sac around the heart. The pain can sometimes feel worse with coughing or taking a deep breath but is usually relieved by sitting up or leaning forward. Pericarditis can also cause the following symptoms:
- Shortness of breath while lying down
- Low-grade fever
- Dry cough
- Abdominal or leg swelling
- Overall sense of weakness or fatigue
Diagnosis of Pericarditis
Several tests are used in the diagnosis of pericarditis, including the following:
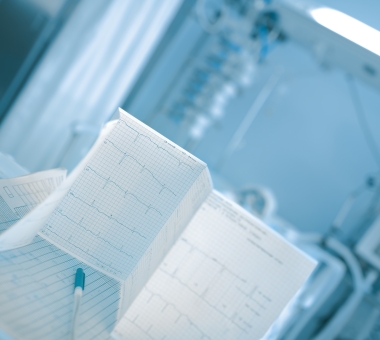
This is the definitive test to assess for the buildup of fluid around the heart. A characteristic sound—called a pericardial rub—may be heard with a stethoscope, though it’s not present if the collection of fluid is large.
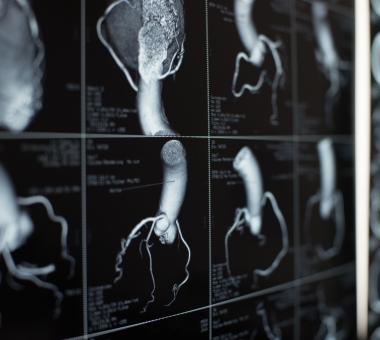
A CT scan uses X-rays to take detailed cross-sectional images of the body, including the arteries and beating heart.

An MRI is a scan that provides pictures of the heart and blood vessels inside the body using a magnetic field and pulses of radio wave energy. Unlike a CT scan, it doesn’t use X-ray radiation. An MRI generates images of the heart and blood vessels, which can help your doctor assess the heart’s structure and function.
Treatment for pericarditis
Pericarditis can range from mild cases that get better on their own to life-threatening cases. It usually lasts less than several weeks, but cases occasionally can last six months or longer. The outcome is generally good if pericarditis is treated promptly. Mild cases of pericarditis may not require treatment. However, if the pericarditis is more severe, treatment is directed at the initial cause for pericardial inflammation.
- Medications – If the pericarditis is caused by an infectious disease, then it’s treated with appropriate medications. Anti-inflammatory medications, such as ibuprofen or steroids, are commonly used as well.
- Fluid drainage – If a large fluid collection (effusion) has developed, drainage of the effusion may be necessary. A surgeon places a drainage tube (catheter) into the sac that surrounds the heart. After the amount of fluid buildup slows down, the catheter is removed.
- Surgery – Occasionally, fluid buildup may reoccur. If this happens, a surgical procedure may be necessary to allow fluid to drain away from the heart. The surgeon cuts away a small piece of the sac (called a pericardial window). If a patient has constrictive pericarditis, which is when the pericardium becomes stiff and acts like a rigid box around the heart, preventing the heart from filling and working properly, treatment may consist of surgery to remove the pericardium, called a pericardiectomy.